A Code Blue procedure is a standardized response to cardiac or respiratory arrest, ensuring rapid activation and effective care to improve patient survival and outcomes.
1.1 Overview of Code Blue
Code Blue is a standardized emergency response system for cardiac or respiratory arrest, ensuring immediate action and coordinated care. It involves rapid identification of life-threatening situations, prompt activation of the Code Blue team, and the delivery of advanced life support measures. The primary goal is to restore normal heart function and breathing as quickly as possible to improve patient survival and outcomes. This system emphasizes a structured approach, including initial assessment, CPR, defibrillator use, and emergency coordination. By standardizing these procedures, healthcare facilities can ensure consistent and effective responses to critical situations, ultimately enhancing patient care and survival rates during medical emergencies.
1.2 Importance of Standardized Code Blue Protocols
Standardized Code Blue protocols are essential for ensuring prompt and effective responses to cardiac or respiratory emergencies. These protocols provide clear guidelines, reducing confusion and delays during critical situations. They ensure that all team members understand their roles and responsibilities, enabling a coordinated effort to save lives. Standardization also improves communication among healthcare providers, patients, and families, ensuring that everyone is aligned in the response process. By adhering to established protocols, healthcare facilities can minimize errors, enhance patient outcomes, and maintain accountability. Ultimately, standardized Code Blue protocols are vital for delivering high-quality, timely care during life-threatening emergencies, making them a cornerstone of hospital emergency preparedness and patient safety strategies.

Definition and Scope of Code Blue
Code Blue is a rapid response system for cardiac or respiratory arrest, ensuring timely medical intervention to improve patient survival and outcomes in healthcare settings.
2.1 What is a Code Blue?
A Code Blue is a standardized emergency response system activated during cardiac or respiratory arrest to ensure immediate medical intervention. It is designed to provide rapid, coordinated care by a trained team to maximize patient survival and outcomes. The Code Blue system is typically triggered when an individual experiences a life-threatening medical emergency, such as cardiac arrest, respiratory failure, or severe physiological instability. Upon activation, a designated Code Blue team, including healthcare professionals, rushes to the location to initiate advanced life support measures, such as CPR, defibrillation, and administration of medications. The primary goal is to restore normal heart function and breathing as quickly as possible to prevent further complications or death.
- Activated by anyone witnessing a cardiac or respiratory emergency.
- Ensures prompt and skilled medical response to life-threatening situations.
- Aims to improve patient survival rates and outcomes through timely intervention.
2.2 Scope of Code Blue Application
The Code Blue procedure applies to all healthcare facilities, ensuring standardized emergency response across various settings. It is primarily implemented in hospitals, clinics, and nursing homes to address life-threatening situations requiring immediate intervention. The scope includes cardiac arrests, respiratory failures, and other critical emergencies that necessitate rapid action. Code Blue protocols are designed to be adaptable, covering both adult and pediatric cases, and are applicable in inpatient, outpatient, and emergency department settings. Activation is not limited to medical staff; patients, visitors, or any witness can initiate the alert if a life-threatening situation arises. This ensures timely assistance and improves patient outcomes by mobilizing resources quickly and effectively.
- Covers all healthcare settings, including hospitals and clinics.
- Addresses cardiac arrest, respiratory failure, and severe emergencies.
- Applicable to both adult and pediatric cases.
- Anyone can activate Code Blue in life-threatening situations.
2.3 Purpose of the Code Blue Team

The Code Blue team is assembled to provide immediate, coordinated, and effective response to life-threatening medical emergencies. Their primary purpose is to assess the situation swiftly, initiate CPR, and use defibrillators or other advanced life-support measures as needed. The team ensures proper airway management, breathing, and circulation to maximize chances of survival. Effective communication and leadership within the team are critical to streamline actions and minimize delays. Additionally, the team collaborates with other hospital departments to facilitate post-emergency care, ensuring seamless patient transfer and ongoing treatment. The Code Blue team also documents the event for legal and quality improvement purposes, while continuously preparing for future emergencies through equipment checks and drills.

- Provides immediate response to life-threatening emergencies.
- Initiates CPR, defibrillation, and advanced life support.
- Ensures effective communication and coordination.
- Facilitates post-emergency patient care and transfer.
- Documents events for legal and quality purposes.

Roles and Responsibilities
Clearly defined roles ensure effective emergency response. The Code Blue team and primary responders collaborate to provide immediate care, following established protocols to save lives.
- Team members execute specific tasks during emergencies.
- Primary responders initiate immediate life-saving interventions.
- Clear communication and coordination are essential.
3.1 Roles of the Code Blue Team Members
The Code Blue team consists of trained healthcare professionals with distinct roles to ensure efficient response during emergencies. Each member’s responsibilities are critical to patient outcomes.
- The team leader coordinates actions, assigns tasks, and oversees the entire response.
- The primary responder initiates CPR and operates the defibrillator.
- Support staff assist with patient positioning, oxygen administration, and equipment preparation.
- Documentation specialists record events, interventions, and outcomes for later review.
Clear role definition ensures seamless collaboration, maximizing the effectiveness of emergency interventions.
3.2 Responsibilities of Primary Responders
Primary responders are the first to arrive at the scene and play a critical role in initiating life-saving interventions. They are responsible for assessing the patient’s condition, verifying cardiac arrest, and starting CPR immediately. Using an automated external defibrillator (AED), they analyze the heart rhythm and deliver shocks as needed. Primary responders ensure high-quality chest compressions, maintaining a depth of 2-3 inches and a rate of 100-120 compressions per minute. They also provide rescue breaths if trained and necessary. Additionally, they administer oxygen therapy and prepare for advanced life support measures. Their prompt actions are vital to preserving neurological function and improving survival chances until the full Code Blue team arrives.

3.3 Notification and Activation Procedures
Notification and activation of Code Blue are critical steps to ensure timely intervention. Upon identifying a cardiac or respiratory emergency, the primary responder must immediately alert the Code Blue team. This is typically done through a hospital-wide paging system, emergency phone, or designated alarm. The responder should clearly state “Code Blue” and provide the location. Simultaneously, they should begin assessing the patient and initiating CPR if necessary. The activation process must be swift and clear to avoid delays. Once activated, the team coordinates their response, with each member understanding their role. Clear communication and adherence to the activation protocol are essential to ensure efficient and effective emergency management. This process is designed to save precious time and improve patient outcomes;

Activation of Code Blue
Activation of Code Blue involves identifying life-threatening emergencies and promptly alerting the response team through designated communication systems to ensure immediate intervention and effective care.
4.1 Identifying a Cardiac or Respiratory Emergency
Identifying a cardiac emergency involves recognizing symptoms like chest pain, sudden collapse, or unresponsiveness, which may signal a heart attack or cardiac arrest. Respiratory emergencies are marked by severe breathing difficulties, such as wheezing, cyanosis, or abnormal breathing patterns. Key signs include loss of consciousness, absence of breathing, or gasping in cardiac cases, and use of accessory muscles, nasal flaring, or blue-tinged extremities in respiratory distress. Assessing the patient’s airway, breathing, and circulation (ABCs) is critical. Medical history, like heart disease or asthma, can aid in differentiation. Utilizing tools such as pulse oximeters or EKGs provides valuable data. Quick identification and effective communication are vital for timely intervention, improving patient outcomes. Continuous training and adherence to protocols enhance accurate assessments and coordinated responses during emergencies.
4.2 Steps to Activate Code Blue
To activate a Code Blue, immediately assess the patient’s condition and confirm the emergency. Call the hospital’s emergency number or press the designated Code Blue button. Clearly state the location and nature of the emergency over the public address system. Ensure trained staff nearby begin CPR if the patient is unresponsive and not breathing. Assign one person to coordinate the response and another to fetch the defibrillator and emergency cart. Notify the on-call Code Blue team and relevant departments. Document the activation time and initial findings. Maintain clear communication to ensure a swift and organized response. The goal is to minimize delays and maximize the chance of a successful outcome.
Implementation of Code Blue Procedure
Implementation involves initiating CPR, using a defibrillator, administering medications, and documenting actions. Coordination and clear communication among team members are crucial for effective execution.
5.1 Initial Assessment and CPR
The initial assessment begins with checking the patient’s responsiveness, airway, breathing, and circulation (ABCs). If unresponsive, not breathing, or without a pulse, CPR should be initiated immediately. Chest compressions are performed at a rate of 100-120 per minute, allowing chest recoil and minimizing interruptions; Rescue breaths are provided if trained, with a ratio of 30:2 for compressions to breaths. Automated External Defibrillators (AEDs) are used to analyze and deliver shocks as needed. CPR continues until advanced life support arrives or the patient regains consciousness. Proper hand placement and technique are critical to ensure effectiveness. All actions are documented for post-event review and patient care continuity.
5.2 Defibrillator Use and ACLS
Defibrillator use is critical in cardiac arrest situations to restore a viable cardiac rhythm. The automated external defibrillator (AED) or manual defibrillator is applied to the patient’s chest via electrodes. The device analyzes the heart rhythm and delivers a shock if ventricular fibrillation or pulseless ventricular tachycardia is detected. Advanced Cardiovascular Life Support (ACLS) protocols are then initiated, including medication administration, rhythm interpretation, and pacing if necessary. ACLS emphasizes high-quality CPR, defibrillation, and pharmacological interventions to maximize the chance of return of spontaneous circulation (ROSC). The team works collaboratively, with clear communication, to ensure timely and effective interventions. Continuous monitoring and adjustments are made based on the patient’s response and ACLS guidelines.
5.3 Coordination of Emergency Response
Effective coordination of emergency response is essential during a Code Blue to ensure a swift and organized approach. The Code Blue team leader directs the effort, assigning tasks and maintaining clear communication. All team members must be aware of their roles and responsibilities to avoid confusion. Communication with hospital staff, security, and other departments is critical to secure the area and manage bystanders. Equipment and personnel are allocated efficiently to maximize response effectiveness. Coordination also involves integrating with the hospital’s emergency response system, ensuring seamless collaboration. This teamwork ensures that interventions are implemented promptly, minimizing delays and improving patient outcomes. Proper coordination is vital for a successful resuscitation effort.
5;4 Documentation During the Event
Accurate and timely documentation during a Code Blue is critical for legal, quality improvement, and patient care purposes. A designated team member, typically not directly involved in patient care, should record all events. This includes the time of cardiac arrest, interventions performed, medications administered, and the patient’s response. Documentation should be concise, clear, and timestamped to provide an accurate record. All defibrillator and monitor data should be saved and included in the patient’s medical record. Post-event, the Code Blue team reviews the documentation to identify areas for improvement. This process ensures transparency, accountability, and better patient outcomes. Standardized forms from the Code Blue checklist can facilitate thorough documentation.
Post-Event Procedures
Debriefing, patient care, and reporting are essential after a Code Blue. The team reviews the event, ensures patient stability, and documents outcomes for future improvements.
6.1 Debriefing and Review
Debriefing and review are critical post-Code Blue steps to improve future responses. A structured discussion, led by a facilitator, involves all team members to reflect on the event. The focus is on identifying successes, areas for improvement, and lessons learned. This blame-free environment encourages open communication. Key topics include patient outcomes, communication effectiveness, and adherence to protocols. Documentation from the event, such as CPR records and witness accounts, is reviewed. Action plans are developed to address gaps. Debriefing also serves as an educational opportunity, reinforcing proper techniques and protocols. It helps the team emotionally process the event, fostering resilience and readiness for future emergencies.
6.2 Patient Care and Transfer
Following a Code Blue event, patient care and transfer are prioritized to ensure continuity of treatment. The primary responder and team assess the patient’s condition post-emergency. If stabilization is achieved, the patient may require transfer to a higher-level care unit or intensive care. Transfer preparation includes securing IV lines, monitoring devices, and ensuring oxygen supply. Communication with the receiving unit is essential to provide detailed handover, including the patient’s status and interventions performed. The healthcare team ensures a smooth transition, updating patient records and maintaining safety during transport. Proper documentation accompanies the patient to facilitate uninterrupted care. This step is vital for optimizing patient outcomes and ensuring all necessary information is communicated effectively.
6.3 Reporting and Documentation
Accurate reporting and documentation are critical after a Code Blue event. All interventions, patient responses, and outcomes must be thoroughly documented. This includes details of CPR, defibrillator use, medications administered, and time-stamped events. Standardized incident report forms are typically used to ensure consistency. Documentation serves as a legal record, aids in quality improvement, and provides insights for future training. The code blue team reviews the event, identifying what went well and areas for improvement. Confidentiality is maintained while ensuring transparency in reporting. Proper documentation also facilitates communication among healthcare teams and supports ongoing patient care. It is essential for accountability and enhancing the effectiveness of future responses.

Training and Preparedness
Regular training and preparedness are essential for effective Code Blue responses. Staff must participate in drills, simulations, and educational sessions to maintain proficiency in CPR, defibrillator use, and emergency protocols. Ongoing education ensures adherence to updated guidelines and improves teamwork. Access to training materials, checklists, and guidelines is critical for preparedness. Continuous learning fosters confidence and competency, enabling healthcare providers to act swiftly and decisively during emergencies.
7.1 Staff Training Requirements
Staff training is critical for effective Code Blue responses. Healthcare personnel must undergo regular training sessions, including theoretical and practical exercises, to master CPR techniques, defibrillator operation, and ACLS protocols. Annual recertification in Basic Life Support (BLS) and Advanced Cardiovascular Life Support (ACLS) is typically required. Training programs should emphasize teamwork, communication, and decision-making under pressure. Simulation drills and real-life scenario exercises are essential to prepare staff for cardiac and respiratory emergencies. Adherence to updated guidelines ensures standardized responses. Proper training fosters confidence, reduces errors, and improves patient outcomes during critical situations. Continuous education and hands-on practice are vital for maintaining proficiency in Code Blue procedures.
7.2 Equipment Familiarization
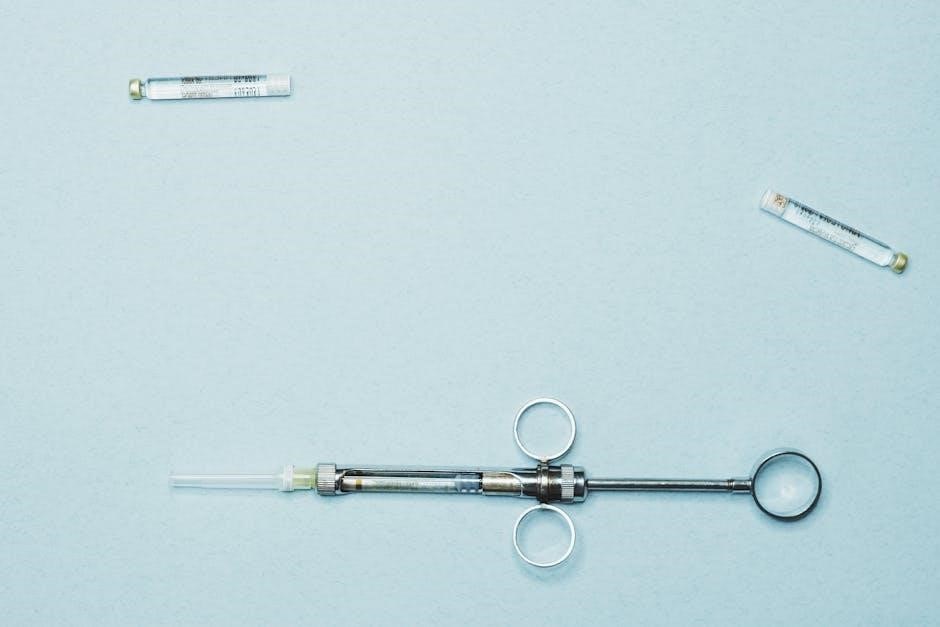
Equipment familiarization is essential for effective Code Blue responses. Staff must be proficient with devices like defibrillators, oxygen tanks, suction machines, and bag-valve-mask (BVM) units. Regular training ensures understanding of equipment operation, maintenance, and troubleshooting. Proper use of defibrillators, including pad placement and shock delivery, is critical. Oxygen therapy equipment must be readily accessible and correctly administered. Familiarity with suction devices helps clear airways efficiently; Staff should also know how to assemble and use BVM devices for ventilatory support. Regular equipment checks and hands-on practice during drills reinforce competence. Ensuring staff are comfortable with Code Blue equipment minimizes delays and improves patient outcomes during emergencies. This preparedness is vital for timely and effective care.
7.3 Regular Drills and Simulations
Regular drills and simulations are vital for ensuring readiness in Code Blue situations. These exercises simulate real-life emergencies, allowing staff to practice protocols, improve response times, and enhance teamwork. Drills should occur quarterly and involve multidisciplinary teams to replicate authentic scenarios. Participants should rotate roles to understand different responsibilities. Debriefing sessions after drills help identify strengths, weaknesses, and areas for improvement. Simulations also familiarize staff with equipment and coordination processes. Timing drills and providing feedback encourage efficiency and accuracy. Regular practice fosters muscle memory and confidence, ensuring staff are prepared to act swiftly and effectively during actual emergencies. This consistent training is key to maintaining high standards of care.
Additional Resources
The Code Blue procedure PDF includes a comprehensive checklist, downloadable guidelines, and contact information for further support. These resources ensure easy access to critical information during emergencies.
They are designed to complement training and serve as quick reference materials for healthcare professionals. Regular updates are provided to reflect the latest protocols.
Accessing these resources helps maintain compliance with established standards and improves response effectiveness. They are essential tools for all Code Blue team members.

8.1 Code Blue Checklist
A Code Blue checklist is a critical tool to ensure efficient and effective response during cardiac or respiratory emergencies. It outlines step-by-step actions for the Code Blue team, including preparation, activation, and execution phases. The checklist typically includes verifying the patient’s identity, assessing the situation, initiating CPR, using a defibrillator, administering medications, and documenting events. It also covers post-event procedures like debriefing and reporting. The checklist is often included in the Code Blue procedure PDF for easy access. Regular reviews and updates ensure it aligns with current guidelines. By following the checklist, healthcare professionals can minimize errors and improve patient outcomes during high-stress situations.
8.2 Downloadable PDF Guidelines

Downloadable PDF guidelines for Code Blue procedures provide a comprehensive and accessible resource for healthcare professionals. These PDFs typically include detailed step-by-step protocols, flowcharts, and checklists to ensure a standardized response during emergencies. They often cover topics such as patient assessment, CPR techniques, defibrillator use, and medication administration. Many organizations offer these guidelines as free downloads, ensuring widespread availability. The PDF format allows for easy printing and sharing, making it a practical tool for training and quick reference. Regular updates are essential to reflect the latest medical advancements and protocol changes. By downloading these guidelines, healthcare teams can ensure they are well-prepared to handle Code Blue situations effectively and efficiently.